
热带病与寄生虫学 ›› 2025, Vol. 23 ›› Issue (2): 110-115.doi: 10.20199/j.issn.1672-2302.2025.02.009
刘世英( ), 李旭芳, 潘火云, 杨花梅, 陈敏霞, 徐翼(
), 李旭芳, 潘火云, 杨花梅, 陈敏霞, 徐翼( )
)
收稿日期:2024-07-11
出版日期:2025-04-20
发布日期:2025-06-04
通信作者:
徐翼,E-mail: 作者简介:刘世英,女,硕士,医师,研究方向:儿童感染性疾病。E-mail:
LIU Shiying( ), LI Xufang, PAN Huoyun, YANG Huamei, CHEN Minxia, XU Yi(
), LI Xufang, PAN Huoyun, YANG Huamei, CHEN Minxia, XU Yi( )
)
Received:2024-07-11
Online:2025-04-20
Published:2025-06-04
Contact:
XU Yi, E-mail: 摘要:
目的 总结儿童中重型广州管圆线虫病临床特点与治疗经验,以期提高对儿童中重型广州管圆线虫病诊疗的认知水平。方法 回顾性分析2018年9月1日—2024年3月30日在广州医科大学附属妇女儿童医疗中心住院的中重型广州管圆线虫病患儿资料,包括一般资料,实验室、影像学及神经电生理检查资料,治疗及预后情况。结果 共纳入18例中重型广州管圆线虫病患儿,其中男性11例,女性7例;年龄中位数为2.2(1.3,4.4)岁。18例患儿均有发热和神经系统症状,5例伴咳嗽、咳痰等呼吸道症状,眼底检查均未查见广州管圆线虫幼虫。患儿外周血嗜酸性粒细胞计数和百分比升高,中位数分别为22.7(14.7,36.0)×109/L和2.3(0.9,4.0)%;脑脊液压力和脑脊液白细胞计数升高,中位数分别为220.0(205.0,272.5) mm H2O和404.0(230.0,841.5)×106/L。14例患儿进行血清广州管圆线虫抗体检测,阳性12例;11例进行脑脊液抗体检测,阳性5例;15例进行脑脊液样本宏基因组测序(metagenomic next-generation sequencing, mNGS),阳性14例;4例进行血液样本mNGS,阳性2例。18例患儿进行头颅MRI检查,16例异常;12例患儿进行胸部CT检查,均有异常。明确诊断后均予以阿苯达唑驱虫治疗,其中16例联合使用糖皮质激素治疗。1例患儿因肺出血死亡;1例有双侧眼球内聚,外展受限;其余16例均治愈,随访1~15月无后遗症。结论 对有发热及神经系统症状、外周血嗜酸性粒细胞增多、头颅MRI或胸部CT提示异常的患儿,应尽早完善寄生虫抗体检测、脑脊液mNGS。广州管圆线虫病早期诊断及早期治疗可有效改善患儿神经系统症状及预后。
中图分类号:
刘世英, 李旭芳, 潘火云, 杨花梅, 陈敏霞, 徐翼. 18例儿童中重型广州管圆线虫病临床特点与治疗分析[J]. 热带病与寄生虫学, 2025, 23(2): 110-115.
LIU Shiying, LI Xufang, PAN Huoyun, YANG Huamei, CHEN Minxia, XU Yi. Clinical pictures and treatment of moderate to severe pediatric angiostrongyliasis in 18 cases[J]. Journal of Tropical Diseases and Parasitology, 2025, 23(2): 110-115.
表1
18例中重型广州管圆线虫病患儿治疗前后外周血及脑脊液实验室检查情况[M(Q1,Q3)]
| 实验室检查 | 驱虫治疗前 | 驱虫治疗第1疗程后 |
|---|---|---|
| 外周血白细胞计数(×109/L) | 9.5(7.8,13.1) | 8.7(7.5,14.0) |
| 外周血EOS计数(×109/L) | 22.7(14.7,36.0) | 7.1(4.8,12.1) |
| 外周血EOS百分比(%) | 2.3(0.9,4.0) | 0.8(0.4,1.1) |
| 外周血血红蛋白(g/L) | 109.0(105.5,119.5) | 116.0(111.0,122.0) |
| 外周血血小板计数(×109/L) | 349.0(315.5,396.5) | 392.0(372.0,552.0) |
| 脑脊液压力(mm H2O) | 220.0(205.0,272.5) | 80.0(68.5,89.0) |
| 脑脊液白细胞计数(×106/L) | 404.0(230.0,841.5) | 121.0(65.0,247.5) |
| 脑脊液氯化物(mmol/L) | 125.1(122.0,127.0) | 124.4(123.2,126.2) |
| 脑脊液葡萄糖(mmol/L) | 2.3(2.0,2.8) | 2.5(2.0,2.8) |
| 脑脊液微量蛋白(g/L) | 0.6(0.5,0.9) | 0.5(0.4,0.6) |
| 脑脊液EOS百分比(%) | 20.0(6.2,34.7) | 0.4(0.0,7.8) |
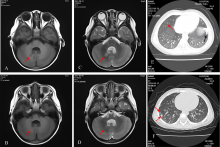
图1
中重型广州管圆线虫病患儿影像学表现 注:A、C为患儿治疗前头颅MRI成像,B、D为患儿治疗后头颅MRI成像,A中右侧小脑半球白质可见一类圆形异常信号影,边界清,T1-TIRM呈稍低信号(红色箭头处);B中T1-TIRM示右侧小脑半球异常强化灶(红色箭头处)较前减小;C中右侧小脑半球白质可见一类圆形异常信号影,边界清, T2-TSE呈稍高信号(红色箭头处);D中T2-TSE示右侧小脑半球异常强化灶(红色箭头处)较前减小。E、F为患儿治疗前胸部CT,E中见双肺支气管血管束增粗、模糊(红色箭头处),双肺下叶可见散在片状、斑片状阴影(黑色箭头处),边缘模糊;F示双肺见多发大小不等结节影,主要位于胸膜下,边缘模糊,可见“晕征”(红色箭头处)。

| [1] | Fuentes I Ferrer MV, Sáez-Durán S, Bueno-Marí R, et al. Health implications of the finding of Angiostrongylus cantonensis,the main cause of eosinophilic meningoencephalitis, in continental Europe (Valencia,Spain)[J]. Rev Esp Salud Publica, 2023, 97:1-6. |
| [2] |
陈家旭, 蔡玉春, 艾琳, 等. 我国重要人体寄生虫病防控现状与挑战[J]. 检验医学, 2021, 36(10):993-1000.
doi: 10.3969/j.issn.1673-8640.2021.010.001 |
| [3] | Cui Y, Shen M, Meng SJ. Lung CT findings of angiostrongyliasis cantonensis caused by Angiostrongylus cantonensis[J]. Clin Imaging, 2011, 35(3):180-183. |
| [4] |
潘火云, 谭丽梅, 徐翼, 等. 12例儿童广州管圆线虫病临床分析[J]. 中国寄生虫学与寄生虫病杂志, 2022, 40(5):668-672.
doi: 10.12140/j.issn.1000-7423.2022.05.016 |
| [5] | 中华人民共和国卫生部. 广州管圆线虫病诊断标准:WS/T 321—2010[S]. 北京: 中国标准出版社, 2010. |
| [6] | 阴赪宏, 甘绍伯, 刘建, 等. 广州管圆线虫病临床诊疗方案(试行)[J]. 临床和实验医学杂志, 2006, 5(10):1473-1474. |
| [7] | 中国疾病预防控制中心寄生虫病预防控制所. 2015年全国人体重点寄生虫病现状调查报告[M]. 北京: 人民卫生出版社, 2018. |
| [8] |
张泽娜, 叶燕芬, 唐屹君, 等. 2017—2019年深圳市寄生虫疑似病例血清学分析[J]. 新发传染病电子杂志, 2021, 6(2):125-128.
doi: 10.19871/j.cnki.xfcrbzz.2021.02.011 |
| [9] | Xie M, Zhou Z, Guo SH, et al. Next-generation sequencing specifies Angiostrongylus eosinophilic meningoencephalitis in infants: Two case reports[J]. Medicine (Baltimore), 2019, 98(35):e16985. |
| [10] | 黄春燕, 刘榆华, 谢汉国, 等. 《广州管圆线虫病诊断标准》(WS/T 321—2010)在福建省和云南省实施情况的跟踪评价[J]. 热带病与寄生虫学, 2024, 22(2):112-116. |
| [11] | Amornpojnimman T, Sanghan N, Ekpitakdamrong N, et al. Angiostrongylosis meningomyelitis without blood eosinophilia[J]. J Infect Dev Ctries, 2021, 15(12):1933-1936. |
| [12] | Jhan KY, Lai GJ, Chang PK, et al. Angiostrongylus cantonensis causes cognitive impairments in heavily infected BALB/c and C57BL/6 mice[J]. Parasit Vectors, 2020, 13(1):405. |
| [13] | 许靖云, 周宇晨, 黄硕, 等. 广州管圆线虫免疫调控机制及诊断技术研究进展[J]. 热带生物学报, 2023, 14(1):60-70. |
| [14] | 周昀, 杨根东. 广州管圆线虫病颅脑及胸部感染一例[J]. 罕少疾病杂志, 2022, 29(1):13-14,29. |
| [15] | Jacob J, Siraj MA, Steel A, et al. Evaluation of the mechanism of action of albendazole on adult rat lungworm (Angiostrongylus cantonensis)[J]. Exp Parasitol, 2022, 242:108355. |
| [16] | 耿艺介, 黄达娜, 高世同, 等. 阿苯达唑治疗广州管圆线虫感染的免疫学效应研究[J]. 寄生虫与医学昆虫学报, 2011, 18(2):70-75. |
| [17] |
Jitpimolmard S, Sawanyawisuth K, Morakote N, et al. Albendazole therapy for eosinophilic meningitis caused by Angiostrongylus cantonensis[J]. Parasitol Res, 2007, 100(6):1293-1296.
doi: 10.1007/s00436-006-0405-7 pmid: 17177056 |
| [18] | 张榕燕, 谢贤良, 方彦炎. 福建省58例广州管圆线虫病分析[J]. 海峡预防医学杂志, 2017, 23(1):27-29. |
| [19] | Evans-Gilbert T, Lindo JF, Henry S, et al. Severe eosinophilic meningitis owing to Angiostrongylus cantonensis in young Jamaican children: case report and literature review[J]. Paediatr Int Child Health, 2014, 34(2):148-152. |
| [20] | Jhan KY, Cheng CJ, Chou CJ, et al. Improvements of cognitive functions in mice heavily infected by Angiostrongylus cantonensis after treatment with albendazole, dexamethasone, or co-therapy[J]. J Microbiol Immunol Infect, 2022, 55(5):935-945. |
| [21] | Jhan KY, Cheng CJ, Jung SM, et al. Co-therapy of albendazole and dexamethasone reduces pathological changes in the cerebral parenchyma of Th-1 and Th-2 dominant mice heavily infected with Angiostrongylus cantonensis: histopathological and RNA-seq analyses[J]. Biomolecules, 2021, 11(4):536. |
| [22] |
刘玉婷, 厉广栩. 儿童重型广州管圆线虫病1例[J]. 中国寄生虫学与寄生虫病杂志, 2022, 40(6):813-816.
doi: 10.12140/j.issn.1000-7423.2022.06.021 |
| [23] | Pham Thu H, Đao Huu N, Thi Thu TL, et al. Case report: Angiostrongylus cantonensis meningoencephalitis in a 9-month-old baby in Vietnam[J]. Am J Trop Med Hyg, 2020, 103(2):723-726. |
| [24] | Liu J, Tao JH, Chen WM, et al. The application of metagenomic next-generation sequencing for Angiostrongylus eosinophilic meningitis in a pediatric patient: a case report[J]. Front Public Health, 2022, 10:1003013. |
| [25] | Tu WC, Lai SC. Angiostrongylus cantonensis: efficacy of albendazole-dexamethasone co-therapy against infection-induced plasminogen activators and eosinophilic meningitis[J]. Exp Parasitol, 2006, 113(1):8-15. |
| [26] | Jacob J, Steel A, Lin Z, et al. Clinical efficacy and safety of albendazole and other benzimidazole anthelmintics for rat lungworm disease (neuroangiostrongyliasis): a systematic analysis of clinical reports and animal studies[J]. Clin Infect Dis, 2022, 74(7):1293-1302. |
| [27] | Chen KY, Cheng CJ, Chen YJ, et al. Protective effect of benzaldehyde combined with albendazole against brain injury induced by Angiostrongylus cantonensis infection in mice[J]. Int J Antimicrob Agents, 2023, 62(5):106963. |
| [28] | Roquini DB, Silva GL, Ferreira LLG, et al. Susceptibility of Angiostrongylus cantonensis larvae to anthelmintic drugs[J]. Front Pharmacol, 2022, 13:901459. |
| [29] | Jacob J, Tan G, Lange I, et al. In vitro efficacy of anthelmintics on Angiostrongylus cantonensis L3 larvae[J]. Parasitology, 2021, 148(2):240-250. |
| [1] | 李知晋, 袁熠, 夏宇, 付晓庆, 漆莉. 2017—2023年重庆市5岁及以下儿童其他感染性腹泻流行特征分析[J]. 热带病与寄生虫学, 2025, 23(1): 12-16. |
| [2] | 张盈, 杨丽蓉, 王晨. 儿童呼吸道合胞病毒感染的临床特征分析[J]. 热带病与寄生虫学, 2024, 22(4): 248-251. |
| [3] | 黄春燕, 刘榆华, 谢汉国, 俞铖航. 《广州管圆线虫病诊断标准》(WS/T 321—2010)在福建省和云南省实施情况的跟踪评价[J]. 热带病与寄生虫学, 2024, 22(2): 112-116. |
| [4] | 王依, 李成媛, 毛元春, 李伟. 基于PRISMA声明的儿童蛲虫病健康教育干预措施的系统综述[J]. 热带病与寄生虫学, 2024, 22(1): 47-53. |
| [5] | 李翔, 付旭文, 许艳玲, 魏佳璐, 杞敏, 干玮, 黄瑛. 儿童并殖吸虫病患者肝脏CT影像学特征分析[J]. 热带病与寄生虫学, 2023, 21(3): 169-173. |
| [6] | 王欣, 贾一博, 王涵, 赵林, 陈亭元, 石卓尔, 闫利春, 薛亚娟. 2021年延安市宝塔区幼儿园儿童蛲虫感染情况调查[J]. 热带病与寄生虫学, 2022, 20(6): 330-332. |
| [7] | 李翔, 付旭文, 耿鹏, 杞敏, 陈海云. 云南省儿童并殖吸虫病临床与影像学特征分析[J]. 热带病与寄生虫学, 2021, 19(6): 316-318,347. |
| [8] | 宋传清, 焦雪成, 黄守梅, 梁桂华, 王兰珍, 朱文刚. 2017—2019 年濮阳市幼儿园儿童蛲虫感染情况调查[J]. 热带病与寄生虫学, 2021, 19(3): 164-166,169. |
| [9] | 张倩, 陈少华, 孙永梅, 陈兆武, 李明. 某肿瘤医院儿童血液病患者 TORCH 感染状况研究[J]. 热带病与寄生虫学, 2021, 19(2): 70-73. |
| [10] | 顾美娟, 刘新华. 广州管圆线虫病 1 例及文献复习[J]. 热带病与寄生虫学, 2021, 19(2): 119-封三. |
| [11] | 郑原印 毛瑛玉 刘晓斌. 儿童阑尾蛲虫感染病理诊断1例[J]. 热带病与寄生虫学, 2019, 17(2): 115-115. |
| [12] | 黄国锋,黄勇,黄焕娣. 广东清远市洲心社区儿童蛲虫病十年防治效果[J]. 热带病与寄生虫学, 2017, 15(4): 226-227,196. |
| [13] | 徐枫,付军,胡本骄,赵正元. 关于留守儿童血吸虫病健康教育策略的几点思考[J]. 热带病与寄生虫学, 2017, 15(4): 236-238,241. |
| [14] | 李天美,陈凤,方文,陈绍荣,李婷,李科荣,刘榆华,罗家军. 2010~2016年大理地区广州管圆线虫病监测病例分析[J]. 热带病与寄生虫学, 2017, 15(3): 167-. |
| [15] | 张王梅,付迎新,赵淑清,杨剑,赵小娟. 511例5岁以下儿童严重急性呼吸道感染流感病毒检测结果分析[J]. 热带病与寄生虫学, 2017, 15(1): 46-47,43. |
| 阅读次数 | ||||||
|
全文 |
|
|||||
|
摘要 |
|
|||||